06 Oct 2017
A summary of Victoria’s 2017 influenza season
Victoria experiences an influenza season each year. Most activity usually occurs between June and September, but the commencement, duration and size of each season varies from year to year. Since 1998 the Victorian Infectious Disease Reference Laboratory (VIDRL) at the Peter Doherty Institute, supported by the Victorian Government Department of Health and Human Services (DHHS), has conducted surveillance for influenza-like illness (ILI) and laboratory confirmed influenza through the Victorian Sentinel Practice Influenza Network (VicSPIN). General practitioners (GPs) report the numbers of total and ILI patients seen each week, and age, sex and vaccination status of ILI patients. GPs collect nose and throat swabs from ILI patients, which are tested by real-time multiplex PCR for influenza A and B and other respiratory viruses at VIDRL. Laboratory confirmed influenza is a notifiable disease in Victoria, for which the DHHS collect data. The National Home Doctor Service (NHDS) operates an out of hours GP service and provides de-identified data to VicSPIN on ILI cases in Victoria. Influenza isolates from VicSPIN are forwarded to the World Health Organization (WHO) Collaborating Centre for Reference and Research on Influenza for antigenic characterisation.
In 2017, 88 GPs participated in VicSPIN from 24 different practices across Victoria. GPs saw a total of 151,951 patients with 1,045 ILI cases, giving an overall proportion of 6.9 ILI cases per 1,000 patients. The median age of ILI cases was 37 years. 510 (49%) were male and 347 (33%) were vaccinated. VicSPIN ILI rates peaked in week ending 24 September at 15.9, slightly above the average seasonal activity threshold (Figure 1) [1]. The NHDS proportion peaked in the week ending 10 September at 51.6 ILI patients per 1,000 consultations, also above the average seasonal threshold.
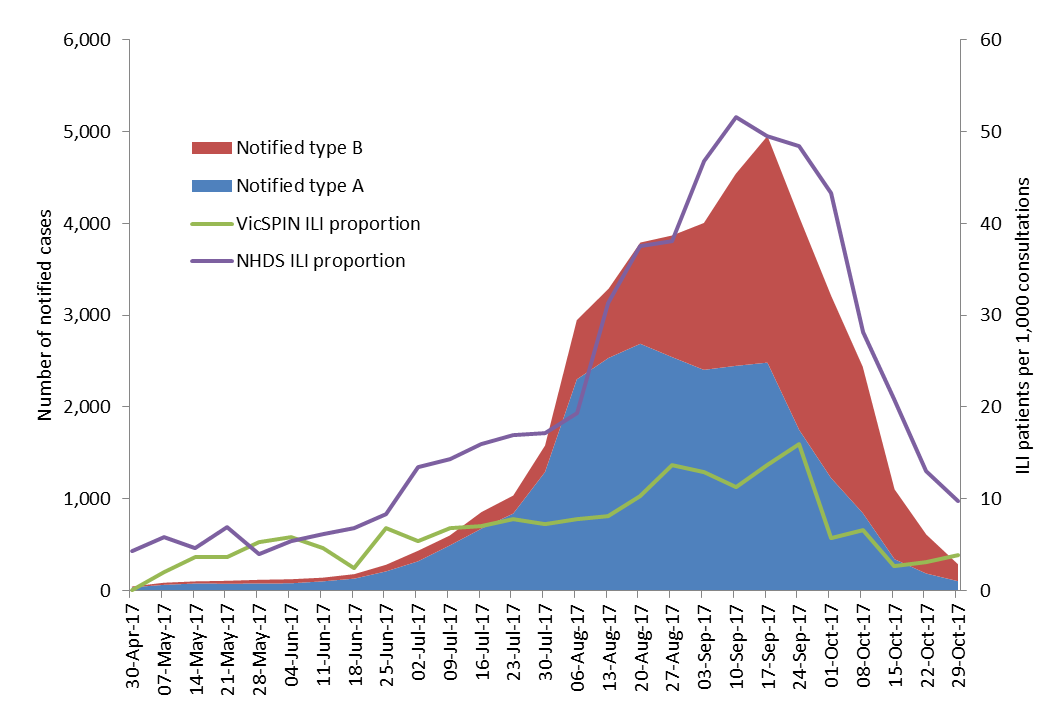
Figure 1. Routinely notified influenza cases and VicSPIN and National Home Doctor Service (NHDS) ILI consultation proportions, Victoria, 2017
VicSPIN received 724 nose and throat swabs during the 2017 season. Of these, 35 were influenza A(H1N1)pdm09, 147 were influenza A(H3), one was influenza A(untyped), and 100 were influenza B. The median ages were 33 years, 40 years and 36 years respectively, reflecting the usual age distribution [2]. Of the total swabbed cases, 214 (30%) were vaccinated, 352 (49%) were male and 116 (16%) had co-morbidities for which influenza vaccination is indicated.
A record number of laboratory confirmed influenza cases (n=47,133) had been notified to DHHS as at 17 December 2017. Higher than average numbers of cases were notified from the start of the year. Influenza type A (identified by VicSPIN as mostly the H3N2 subtype) was predominant at the start of the season, with an increase in influenza type B towards the end of the season. Overall, 60% and 40% of notified influenza cases were type A (median age 41 years) and type B (median age 37 years) respectively.
Data from swabbed VicSPIN ILI patients contribute to the calculation of annual national influenza vaccine effectiveness estimates. Overall vaccine effectiveness for the 2017 influenza vaccine was calculated to be 33% (95%CI: 17 to 46) [3]. Vaccine effectiveness was lower against influenza A(H3) infection (10% (95%CI:-16 to 31) and higher for A(H1N1)pdm09 (50%; 95%CI: 8 to 74) and type B (57%; 95%CI: 41 to 69) infections [3].
Authors: Kristina Grant (VIDRL), James Fielding, Kylie Carville, Janet Strachan DHHS


